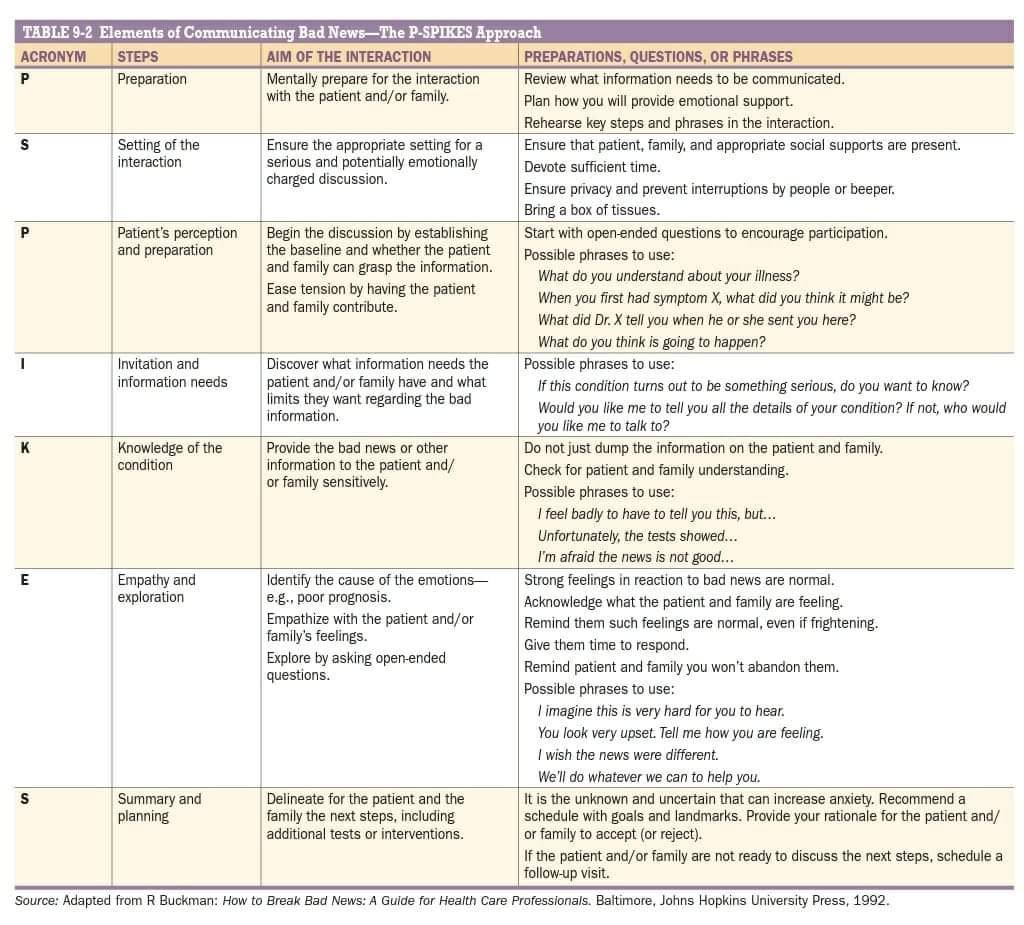
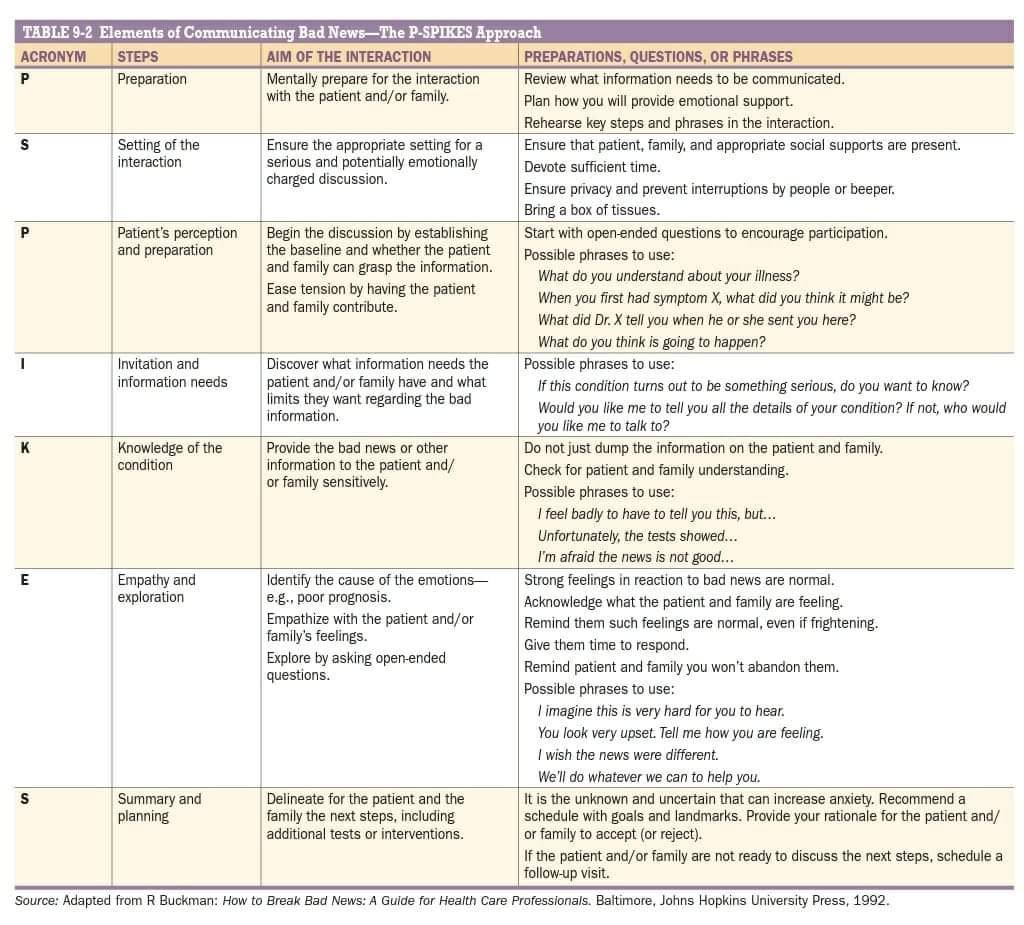
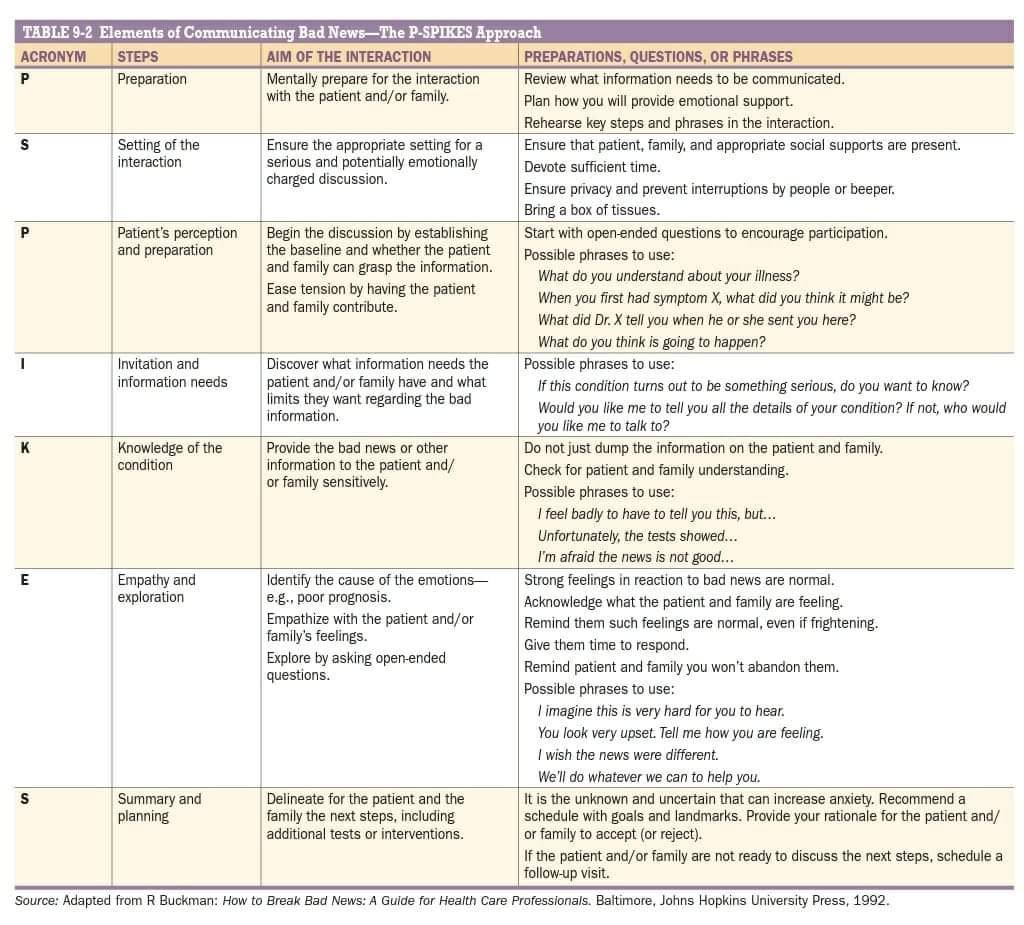
Sharing the Bad News – P-SPIKES Approach
Apart from using PPE kit, isolation and hand hygiene, following should be done to minimize risk while handling patient of any suspected COVID-19 pneumonia on ventilator .

Top 100 secrets in critical care medicine
1. Elevated lactate levels suggest tissue hypoperfusion, and normal lactate clearance is
suggestive of adequate fluid resuscitation.
2. Always assume that even a single episode of hypotension in a trauma patient is due tobleeding, and proceed accordingly.
3. Good cardiopulmonary resuscitation can make a difference for a successful resuscitation from cardiac arrest. Know and perform it well.
4. Time to defibrillation is the most important factor in a return of spontaneous circulation from ventricular tachycardia and/or ventricular fibrillation.
5. Pulse oximetry is good for continuous monitoring, but arterial blood gases (ABGs) are best for diagnosis and acute management. If oximetry does not fit the clinical picture,obtain an ABG.
6. Use the alveolar gas equation to help understand mechanisms of hypoxemia.
7. Hemodynamic monitoring assesses whether the circulatory system has adequate performance to supply oxygen and sustain the “fire of life.” Monitoring provides data to guide therapy but is not therapeutic.
8. There is no proved benefit to colloid over crystalloid in acute resuscitation.9. Starting enteral nutrition early in critically ill patients increased survival.
10. Enteral feeding in patients with shock is acceptable after the patient is resuscitated and hemodynamically stable, even if the patient is receiving stable lower doses of
vasopressors.
11. The primary indications for mechanical ventilation are inadequate oxygenation, inadequate
ventilation, and elevated work of breathing.
12. Low tidal volume mechanical ventilation can lead to improved outcomes in the patient withacute respiratory distress syndrome.
13. Daily weaning assessments improve patient outcomes.
14. The rate of central venous catheter–related bloodstream infections can be reduced through a combination of the use of maximal sterile barrier precautions, 2% chlorhexidine-based antiseptic, centralization of line insertion supplies, and daily evaluation of the need for continued central access.
15. Subclavian venous catheters have the lowest risk of bloodstream infection.
16. Lung sliding on ultrasound examination effectively rules out pneumothorax at the site of the transducer.
17. Extracorporeal membrane oxygenation can be used successfully in patients with respiratory failure in whom low tidal volume ventilation is failing.18. Nonrecognition of an esophageal intubation leads to death; direct visual confirmation or detection of carbon dioxide must be done to confirm the proper location of an endotracheal tube.19. If a tracheostomy tube falls out of its stoma within the first 1 to 5 days of placement, do not attempt to reinsert it blindly. Perform translaryngeal intubation instead because blind attempts at reinsertion misplace the tube into a paratracheal track, compress the trachea,and cause asphyxia.20. Any airway or stomal bleeding that develops more than 48 hours after tracheotomy should suggest the possibility of a tracheoarterial fistula, which develops as a communication between the trachea and a major intrathoracic artery.
21. A retrospective study showed that positive pressure ventilation (PPV) does not influence the rate of recurrent pneumothorax or chest tube placements after removal. Consequently, presence of mechanical PPV is not anindication to leave a chest tube in place.22. Chest physiotherapy appears to be as effective as bronchoscopy in treating atelectasis, although bronchoscopy has a role in retained, inspissated secretions or foreign bodies.23. Pulmonary artery line placement in patients with a newly implanted (less than 3 months)implantable cardioverter defibrillator or pacemaker is associated with high risk of lead dislodgment, especially if there is a coronary sinus lead.24. Intraaortic balloon pumps should be considered in patients who may benefit from increased diastolic pressures (persistent refractory angina, cardiovascular compromise from myocardial ischemia/infarction) or decreased afterload (acute mitral regurgitation,cardiogenic shock).25. Clinical judgment should supplement severity of illness scores in defining patients with severe community-acquired pneumonia.26. The use of clinical criteria alone will lead to the overdiagnosis of ventilator-associated pneumonia.27. A normal PCO2 in acute asthma is a warning sign of impending respiratory failure.28. Noninvasive mechanical ventilation reduces the need for intubation in patients with achronic obstructive pulmonary disease exacerbation and impending respiratory failure.
29. Chronic hypoxemia is the most common cause of pulmonary hypertension.30. Patients with acute lung injury and acute respiratory distress syndrome die of multiorgan dysfunction far more frequently than they do of refractory hypoxemia.
31. For most patients, bronchial artery embolization is the treatment of choice to stop hemorrhaging in massive hemoptysis. 32. Because death from massive hemoptysis is more commonly caused by asphyxiation than
exsanguination, it is important to emergently maintain airway patency and protect the
nonbleeding lung.33. Deep venous thrombosis and pulmonary embolism are common and often
underdiagnosed in critically ill patients.34. The key to treating heart failure is determining the cause, that is, reduced ejection fraction,normal/preserved ejection fraction, restrictive cardiomyopathy, hypertrophic cardiomyopathy, or right ventricular failure.35. The best clinical guide to help in choosing which treatment is appropriate for the critically ill patient with heart failure is to assess volume and perfusion status.36. Acute myocardial infarction, complicated by out-of-hospital cardiac arrest, has a very high mortality, and hypothermia may improve chances for survival and neurologic recovery.37. It is important to distinguish hemodynamically unstable arrhythmias that need immediate cardioversion/defibrillation from other more stable rhythms.38. When managing acute aortic dissection, adequate beta blockade must be established before the initiation of nitroprusside to prevent propagation of the dissection from a reflex increase in cardiac output.39. Pulsus paradoxus is when there is respiratory variation on arterial waveform seen during pericardial tamponade of >10 mm Hg.40. Severe sepsis ¼ sepsis plus acute organ dysfunction.
41. Early diagnosis and therapeutic interventions in patients with severe sepsis or septic shock
are associated with better outcomes.42. Between 60% and 80% of cases of endocarditis result from streptococcal infection.Staphylococcus aureus tends to be the most common etiologic agent of infective endocarditis in intravenous (IV) drug users.43. Streptococcus pneumoniae remains the most common cause of community-acquired
bacterial meningitis, and treatment directed to this should be included in the initial empiric regimen.44. Most patients do not require computed tomographic scan before lumbar puncture;however, signs and symptoms that suggest elevated intracranial pressure should prompt imaging. These include new-onset neurologic deficits, new-onset seizure, and papilledema. Severe cognitive impairment and immune compromise are also conditions that warrant consideration for imaging.45. If you suspect disseminated fungal infection, do not wait for cultures to treat.
46. Reducing multidrug-resistant bacteria can only be accomplished by using fewer antibiotics, not more.47. Clinical or laboratory identification of an unusual pathogen (i.e., anthrax, smallpox, plague) should raise suspicion for a biologic attack.48. Pain disproportionate to physical findings; skin changes including hemorrhage, sloughing, or
anesthesia; rapid progression; crepitus; edema beyond the margin of erythema; and systemic involvement should prompt intense investigation for deep infection and involvement of surgical consultants as needed in the case of necrotizing fasciitis or gas gangrene.49. During influenza season all persons admitted to the intensive care unit (ICU) with respiratory illness should be presumed to have influenza and be tested and treated.50. Asplenic individuals are at risk for infection with encapsulated organism.
51. The greatest degree of immunosuppression in solid organ transplant recipients is in the 1
to 6 months after transplantation.52. Severe hypertension in absence of end organ damage can be safely treated outside the setting of intensive care and reduction in blood pressure be achieved gently over hours to days.53. The serum creatinine level may not change much during acute renal failure in patients with decreased muscle mass.
54. In the analysis of acid-base disorders, a normal serum pH does not imply that there is not an acid-base disorder; rather it points to mixed disorder.55. Serum magnesium level should be checked and corrected, if low, in patients with refractory hypokalemia.56. Overly rapid correction of hyponatremia or hypernatremia can result in devastating
long-term neurologic sequelae.57. If a patient has neurologic symptoms associated with hyponatremia, one of the immediate goals of therapy should be correction of serum sodium to a safe level.58. Be systematic in your workup of gastrointestinal tract bleeding. Follow an algorithm.59. In a patient with acute pancreatitis, make sure the patient’s fluid is replenished with an adequate amount of IV fluid. This is as important as, if not more important than, the other facets of treatment, including pain control, nutritional support, correcting electrolyte abnormalities, treating infection (if present), and treating the underlying cause.60. Steroids should be considered for the treatment of severe alcoholic hepatitis as defined by a Maddrey’s discriminate score 32.
61. Abdominal compartment syndrome is an underappreciated diagnosis.62. This is no secret—we all share the responsibility for reducing nosocomial infections.63. Worsening confusion or a new impairment in mental state during treatment of diabetic ketoacidosis or hyperosmolar hyperglycemic state is life-threatening cerebral edema until proved otherwise. 64. Administering insulin without adequate fluid replacement during treatment of diabetic ketoacidosis or hyperosmolar hyperglycemic state can lead to profound hypotension,shock, or cardiovascular collapse.65. An IV insulin infusion is the safest and most effective way to treat hyperglycemia in critically
ill patients.66. If the blood pressure of an ICU patient with septic shock responds poorly to repeated fluid boluses and vasopressors, hydrocortisone should be given regardless of cortisol levels.67. In most cases you do not need to treat nonthyroidal illness syndrome with levothyroxine despite low thyroxine, triiodothyronine, and thyroid-stimulating hormone levels; instead follow expectantly, and recheck laboratory values in 4 to 6 weeks.68. Stable anemia is well tolerated in critically ill patients. Transfuse blood products only when necessary or if hemoglobin level drops below 7 gm/dL.69. Although disseminated intravascular coagulation typically presents with bleeding or
laboratory abnormalities suggesting deficient hemostasis, hypercoagulability and accelerated thrombin generation actually underlie the process.70. Surgery for cord compression can keep people ambulatory longer than radiation alone.
71. For a neutropenic fever, draw cultures, give broad-spectrum antibiotics, then complete the workup.72. In a patient in the ICU who is seen with multiorgan failure or a clinical picture resembling fulminant sepsis, consider the diagnosis of systemic lupus erythematosus or vasculitis.73. Respiratory pattern, autonomic functions, and brain stem reflexes are critical in identifying the cause of coma and should be recorded in all patients.74. No ancillary test can replace an experienced clinical examination for determination of brain death.75. The mainstay of treatment for status epilepticus includes stabilizing the patient, controlling the seizures, and treating the underlying cause.
76. ICU admission, invasive hemodynamic monitoring, and respiratory support with frequent vital capacity measurements are keys to following patients with Guillain-Barre´ syndrome.77. Tachypnea is often the first sign of respiratory muscle weakness. Respiratory muscle strength is ideally measured by maximum inspiratory flow and vital capacity (VC) in patients with myasthenia gravis. A quick surrogate for forced VC is to ask the patient to
count to the highest number possible during one expiration.78. Benzodiazepines are the preferred agents for the treatment of alcohol withdrawal.79. Time should not be wasted pursuing radiographic confirmation when a tension
pneumothorax is suspected in a hemodynamically unstable patient. Either formal tube thoracostomy should be immediately performed or an Angiocath inserted into the second intercostal space along the midclavicular line.
80. The condition of a significant number of patients with flail chest and/or pulmonary contusion can be safely and effectively managed without intubation by using aggressive pulmonary care, including face-mask oxygen, continuous positive airway pressure, chest physiotherapy, and pain control.
81. The model for end-stage liver disease (MELD) calculates the severity of liver disease.82. Delirium is a disturbance of consciousness with inattention, accompanied by a change in cognition or perceptual disturbances that develop over a short period of time, fluctuate over days, and remain underdiagnosed.83. Therapeutic hypothermia (temperature 30 -34 C) improves neurologic outcomes in comatose survivors of cardiac arrest.84. Heat stroke is a true medical emergency requiring immediate action: Delay in cooling increases mortality.85. When caring for a critically ill poisoned patient, the diagnostic and therapeutic interventions should be started on the basis of the clinical presentation, with use of the history, the physical examination, and recognition of toxidromes.86. Syrup of ipecac and gastric lavage have no role in the routine management of the poisoned patient.87. Oral or IV N-acetylcysteine should be administered promptly to any patient with suspected or confirmed acetaminophen toxicity.
88. Patients with methanol and ethylene glycol ingestions present with an osmolal gap, which closes with metabolism and develops an anion gap acidosis. Isopropanol toxicity begins with an osmolal gap but is not metabolized to an anion gap.89. Patients with toxic alcohol ingestion and any vision disturbance, severe metabolic acidosis,or renal failure should undergo urgent hemodialysis.90. The treatment of choice for calcium channel blocker toxicity is hyperinsulinemiaeuglycemia therapy to maximize glucose uptake into cardiac myocytes.
91. Neuroleptic malignant syndrome can occur at any age in either sex with exposure to any antipsychotic medication.92. Although radiologic investigations and drug treatment may carry some risk of harm to the fetus, necessary tests and treatment should not be avoided in the critically ill mother.93. Patients and their families are the experts on the patient’s goals and values, and clinicians are the experts on determining which clinical interventions are indicated to try to achieve reasonable clinical goals.94. Timely ethics consultation in the ICU may mitigate conflict and reduce ICU length of stay,hospital length of stay, ventilator days, and costs.95. Only discuss treatment choices after the patient or family has been updated on medical condition, prognosis, and possible outcomes and once overall goals of medical care are agreed on.96. Family conferences are more successful when providers listen more and talkless. Encourage the family to discuss their understanding of illness, their emotions,
and who the patient is as a person. Then respond with statements of support and understanding.97. All patients with impending brain death or withdrawal of care should be screened for the possibility of organ donation.98. The gap between those patients awaiting a transplant and those donating organs is widening exponentially—the vast majority of those on the transplant list will die waiting.99. The hospital systems investing today in advanced informatics, automated decision analysis, telemedicine, and/or regionalized care will be the leading systems tomorrow.
100. Patient safety remains a concern in critically ill patients, and a primary barrier to improving patient safety is physicians’ inability to change their practice patterns.
Symbols used on ABG report and the Seven Step approach to ABG analysis
Normal Arterial Blood Gas Values
pH 7.35-7.45
PaCO2 35-45 mm Hg
PaO2 70-100 mm Hg**
SaO2 93-98%
HCO3- 22-26 mEq/L
MetHb <2.0%
COHb <3.0%
Base excess -2.0 to 2.0 mEq/L
CaO2 16-22 ml O2/dl
** Age-dependent
Symbols used on the ABG Reports
—–
∎ pH(a)-
pH is the negative logarithm of the hydrogen ion activity (pH = – logaH+)
pH stands for ‘potential of hydrogen’
Reference range (adult): 7.35 – 7.45
Reference range (pediatric) 7.27-7.47
—–
∎pCO2(a)
Carbon dioxide partial pressure
pCO2 in atmosphere 0.3 mmHg (can be considered as zero in comparison to expired air. Therefore, pCO2 is a direct reflection of the adequacy of alveolar ventilation in relation to the metabolic rate
pCO2 inversely proportional to the alveolar ventilation
PaCo2= VCO2x 0.863/ VA
—–
∎ctCO2(P)c
Carbon Dioxide content of Blood
Normal Value Arterial Blood- 21.5mmol/L (48ml/dl)
Normal Value Mixed Venous Blood- 23.5mmol/L (52 ml/dl)
Only PCO2 is measured. HCO3 and CtCO2 is calculated from pCO2 and pH of the sample.
ctO2 = (tHb x 1.36 x F O2Hb) + (Po2 x 0.003)
mmHg to kPa conversion factor – multiply by 7.5
—–
∎pO2- partial pressure of oxygen
Analytical methods for measuring oxygen saturation arterial blood gas analyzers
1. pulse oximetry
2. CO-oximetry
Oxygen saturation
SpO2 noninvasively by pulse oximetry
SaO2 Arterial blood gas analyzers calculate estimated oxygen saturation (O2sat) in a blood sample based on empirical equations using pH and PO2 values.
Co-Oximeter like the reports in the example directly measure SaO2 and therefore accurate.
—–
p50
It is defined as the partial pressure of oxygen at which the oxygen carrying protein is 50% saturated
The P50 of normal adult haemoglobin is 26.6 mmHg.
—–
cHCO3–(act)
cHCO3– is the concentration of bicarbonate (hydrogen carbonate) in the plasma of the sample.
It is calculated using the measured pH and pCO2 values.
The analyzer symbol cHCO3–(act).
—–
What does cHCO3– tell you?
The actual bicarbonate is calculated by entering the measured values of pH and pCO2 in the Henderson-Hasselbalch equation.
Ka is the dissociation constant of the weak acid, pKa = log Ka, and [HA] and [A] are the molarities of the weak acid and its conjugate base.
—–
∎cHCO3–(std) Standard bicarbonate
Concentration of hydrogen carbonate in plasma from blood which is equilibrated with a gas mixture with pCO2= 40 mmHg (5.3 kPa) and pO2 100 mmHg (13.3 kPa) at 37 °C
Eliminates the respiratory component in the acid base status
Low standard bicarbonate indicates a metabolic acidosis, and an elevated standard bicarbonate indicates a metabolic alkalosis.
∎Base Excess
Quantity (milliequivalent) of acid needed to titrate 1 L of blood to pH 7.4 at Temp 37C and PaCO2 40 mmHg.
Assessment of the metabolic component of acid base disorders
In contrasted to the bicarbonate levels, the base excess is a calculated value intended to completely isolate the non-respiratory portion of the pH
Two types
Blood – BE(b)
Extra cellular fluid – BE(ecf)
∎ There are two calculations for base excess:
BE(b) = (1 − 0.014 x hgb) x (cHCO3 − 24.8 + (1.43 x hgb + 7.7) x (pH −7.4)
BE(ecf) = cHCO3 − 24.8 +16.2 X (pH −7.4)
—–
∎ BE (B) [Blood] [Actual]
Actual base excess is the concentration of titratable base when the blood is titrated with a strong base or acid to a plasma pH of 7.40 at a pCO2 of 40 mmHg (5.3 kPa) and 37 °C at the actual oxygen saturation.
Buffer base represents the Total Buffer Capacity in the blood, comprised of bicarbonate, hemoglobin, plasma proteins and phosphate
—–
∎ BE (ecf) [Standard]
Standard base excess is an in vivo expression of base excess
Standard base excess is the value when the Hemoglobin is at 5 g/dl
It refers to a model of the extra cellular fluid (one part of the blood is diluted by two parts of its own plasma) and is calculated using one third of the ctHb for blood in the formula
∎ What does cBase(Ecf) tell you?
cBase(Ecf) is the base excess in the total extracellular fluids, of which blood represents approximately one third. Buffering capacities differ in the extra-cellular compartments, which makes the cBase(Ecf) more representative of the in vivo base excess compared to actual BE(b).
Example: Base deficit with elevated anion gap indicates addition of acid (e.g., ketoacidosis)
Base deficit with normal anion gap indicates loss of bicarbonate (e.g., diarrhea). The anion gap is maintained because bicarbonate is exchanged for Chloride during excretion.
—–
∎ pO2(A-a) Alveolar/Arterial Gradient
Alveolar/Arterial Gradient Alveolar Po2 = [(barometric pressure – water vapor pressure) × Fio2] – [1.25 × Pco2]- PaO2
—–
∎ pO2 a/A Arterial/Alveolar Oxygen Ratio
The arterial/alveolar (a/A) ratio= PaO 2 /PA o 2
The A/a gradient increases as the concentration of oxygen the patient inspires increases.
The a/A ratio is not dependent on Fio2 (Normal Range 0.8 to 0.9, 0.75 in the elderly)
Low a/A ˂ 0.6 indicates Shunt, V/Q mismatch or diffusion defect,
˂ 0.35 weaning failure
˂ 0.15 Refractory hypoxemia
—–
Co-Oximetry
Hct Fraction of the volume of erythrocytes in the volume of whole blood
tHb Total hemoglobin
sO2 Oxygen saturation of hemoglobin
FO2Hb Fraction of oxyhemoglobin in total hemoglobin in blood
FCOHb Fractional carboxyhemoglobin
FMetHb Fractional Methemoglobin
FHHb Fractional Deoxyhemoglobin
—–
—–
∎ BO2 (Oxygen capacity of hemoglobin) The maximum concentration of oxygen bound to hemoglobin in blood, saturated so that all deoxyhemoglobin is converted to oxyhemoglobin
ctO2(a) (Total content of oxygen in the arterial blood)
Electrolytes
Na+ Sodium concentration
K+ Potassium concentration
Ca++ Calcium concentration
Ca++(7.4) Calculated value of ionized calcium at pH 7.4
Cl- Chloride concentration
AnGap Unmeasured anions in the plasma
Anion GapC Na- Cl-HCo3
Anion Gap(K+) Na+K-Cl-HCO3
Metabolites
∎ Glucose(Concentration of glucose in plasma)
As both hyper and hypoglycemia can produce neurological damage, aggressive treatment of deviations in cGlu is warranted.
—–
Lactate (L-Lactate)
Lactate(P) is the concentration of lactate in plasma
D-lactic acidosis Isomer produced by gut flora occur in patients with short bowel syndrome
D-lactate are not found in healthy individuals
L-lactic acid Isomer produced by humans and the acid responsible for lactic acidosis
ABG machines measure only L Lactate
Lactate- A marker for sepsis and Trauma
Lactate is used as an indicator of impaired metabolism in trauma and sepsis patients may help emergency caregiver’s further diagnosis, risk stratify, and treat patients in the ED
Rising levels of lactic acid are associated with increased mortality independent of degree of organ dysfunction and shock at presentation
Lactic Acid Clearance=
Initial lactate – subsequent lactate/initial lactate × 100
—–
∎mOsmc
Plasma osmolality & osmolarity
Osmolality- osmolality (with an “ℓ”) is a measure of the osmoles (Osm) of solute per kilogram of solvent (osmol/kg or Osm/kg)
Osmolarity (with an “r”) is defined as the number of osmoles of solute per liter (L) of solution (osmol/L or Osm/L).
Mnemonic- Remember the word R for Liter
Osmolarity is affected by changes in water content, as well as temperature and pressure
In practice, there is almost negligible difference between the absolute values of the different measurements.
Both terms are often used interchangeably
Calculated osmolarity = 2 Na + 2 K + Glucose + Urea (all in mmol/L).
To calculate plasma osmolarity use the following equation : = 2[Na+] + [Glucose]/18 + [ BUN ]/2.8 where [Glucose] and [BUN] are measured in mg/dL.
————–
Seven Step Approach To The Diagnosis Of An ABG
First Check whether the report is reliable
H+ =24X CO2/HCO3
pH Approximate H+ concentration
7.60 25
7.55 28
7.50 32
7.45 35
7.40 40
7.35 45
7.30 50
7.25 56
7.20 63
7.15 71
Acid Base Status
Step 1 Look for pH Acidemic pH < 7.4
Alkalemic pH > 7.4
Step 2 Look for CO2 and HCO3
Is main disturbance metabolic or respiratory?
Step 3 If the primary disorder is respiratory, is it acute or chronic
ΔpH= 0.008 x Δ PCO2 (Acute)
ΔpH= 0.003 x Δ PCO2 (chronic)
Sometimes pH can be markedly altered due to other disorders
Acute hypercapnia Δ H+ / ΔPaCO2 > 0.7
Chronic hypercapnia Δ H+ / Δ PaCO2 < 0.3
Step 4 Calculate renal compensation to determine the metabolic deviation due to respiratory disorder
For acidosis
Early (6-24 hours) ΔHCO3= 1/10 X ΔPCO2
Late (1-4 days) ΔHCO3= 4/10 x ΔPCO2
For alkalosis
Early ΔHCO3= 2/10 X ΔPCO2
Late (2days) ΔHCO3= 5/10 x ΔPCO2
Decide- If not there is superimposed metabolic disturbances or the compensation is not yet complete
Step 5 If there is a metabolic acidosis is the Anion gap increased.
Determine the AG and narrow down your diagnosis
Step 6 If there is a metabolic disturbance is there appropriate respiratory compensation
Metabolic acidosis (Winters formula)
Expected PaCo2= 1.5(HCO3)+ 8
Metabolic alkalosis
Expected PaCO2= 0.7(HCO3)+21
Step 7 Diagnosis of mixed acid base disorder
If anion gap is increased >20 there is an high anion gap acidosis
Is there a non anion gap acidosis?
1. Gap-Gap Δ AG/ Δ HCO3
If less than 1 there is a superimposed non anion gap metabolic acidosis
If more than 1.6 there is a superimposed metabolic alkalosis
2. Calculate Excess Anion Gap [HCO3 + (Anion gap-12)] = 24
If this value is less than 24 there is a hidden non anion gap acidosis
If this value is more than 24 then there is a metabolic alkalosis hidden in the numbers
3. Bicarbonate gap
Δ AG- ΔHCO3= (Na-Cl-HCO3)-12—(27-HCO3)
Na-Cl-39
If Bicarbonate gap is more than +6 there is a metabolic alkalosis hidden in the numbers
If Bicarbonate gap is less than – 6 then there is a metabolic acidosis hidden in the numbers
Oxygenation
PaO2
SaO2
CaO2
Ventilation
PaCO2
http://www.ncbi.nlm.nih.gov/pubmed/25510301
Important differences in epidemiology of candidemia in Indian ICU :
1. High incidence
2. Younger patients (49.7 yr)
3. Early infection (11 days median)
4. Lower Apache score (17.2)
5. Azole resistance (11.8% , MDR 1.9%)
6. High mortality (40℅, Attributable 23%)
7. Vast spectrum (31 spectrum)
1. Ventilator-associated pneumonia in the ICU.Crit Care. 2014;18(2):208.
Link: http://download.springer.com/static/pdf/721/art%253A10.1186%252Fcc13775.pdf?originUrl=http%3A%2F%2Fccforum.biomedcentral.com%2Farticle%2F10.1186%2Fcc13775&token2=exp=1459489177~acl=%2Fstatic%2Fpdf%2F721%2Fart%25253A10.1186%25252Fcc13775.pdf*~hmac=9505a0c1d79f95a259588425bc727721aa97768119a4f2e9230af2f461d5944e
2. Hospital-acquired pneumonia, health care-associated pneumonia, ventilator-associated pneumonia, and ventilator-associated tracheobronchitis: definitions and challenges in trial design. Niederman MS. Clin Infect Dis.2010; 51(S1):S12–S17.
Link: http://cid.oxfordjournals.org/content/51/Supplement_1/S12.full.pdf
3. Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia, Am J Respir Crit Care Med Vol 171. pp 388–416, 2005
Link: http://www.atsjournals.org/doi/pdf/10.1164/rccm.200405-644ST
4. Recommendations for treatment of hospital-acquired and ventilator-associated pneumonia: review of recent international guidelines. Clinical Infectious Disease. 51(Suppl 1):S42–7.
Link: http://www.wzhealth.com/upload/201412/09/201412091419583046.pdf
5. Ventilator-associated pneumonia. Current OpinCrit Care 2009;15: 30–5.
Link: http://master.pneumologia-interventistica.it/materiale/fontanari/current%20opin%20crit%20care%202009.pdf
6.Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society
http://m.cid.oxfordjournals.org/content/early/2016/07/06/cid.ciw353.full
Slideshare (PDF) :
http://www.slideshare.net/vitrag24/ventilatory-management-of-acute-hypercapnic-respiratory-failure
Mediafire (PPT) :
https://www.mediafire.com/?36hj6kjgb7t8o3g
Mediafire link (Download articles & BTS guideline) :
https://www.mediafire.com/?7lpc809cheji59x
Principles and Procedures for Blood Cultures Clinical and Laboratory Standards Institute No 47A Vo l27 No17
Link: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185849/
Blood Cultures in the Critical Care Unit: Improving Utilization and Yield. Chest 122:1727-1736
Link: http://journal.publications.chestnet.org/pdfaccess.ashx?ResourceID=2106155&PDFSource=13
Typhoid Fever. New Engl J Med 2002;347:1770-82.
Link: http://www.nejm.org/doi/full/10.1056/NEJMra020201
Meta Analysis: Methods for Diagnosing Intravascular Device Related Blood Stream Infections. Ann Intern Med 2005:142:451-466
Link: http://annals.org/article.aspx?articleid=718270
Multiplex Real-Time PCR and Blood Culture for Identification of Bloodstream Pathogens in Patients with Suspected Sepsis. Clinical Microbiology and Infection Volume 15, Issue 6, June 2009, Pages 544–551
Rapid Molecular Detection of Tuberculosis and Rifampin Resistance. New Engl J Med 2010 ; 363 : 1005-1015
Link: http://www.nejm.org/doi/pdf/10.1056/NEJMoa0907847
Review of Rapid Diagnostic Tests Used by Antimicrobial Stewardship Programs, Clinical Infectious Diseases 2014;59(S3):S134–45
Link: http://cid.oxfordjournals.org/content/59/suppl_3/S134.full.pdf+html
🤔MEASUREMENT OF CORE BODY TEMPERATURE: FAQs
❓What’s the problem, if we place the temperature probe in upper 1/3rd or 2/3rd of the esophagus?
✔️Esophageal temperature should be taken from the lower third of the oesophagus; placed above this level, the probe may under-read due to cooling effect of inspired gases. It gives a good estimate of cerebral blood temperature.
❓What’s the advantage of nasopharyngeal temperature measurement over oesophageal measurement?
✔️The nasopharyngeal temperature probe is placed just behind the soft palate. The advantage is that it is more accessible compared to the oesophageal temperature measurement. The disadvantage is that it is less accurate in representating the core temperature.
❓What are the advantages of measurement of temperature @ Tympanic membrane?
✔️The tympanic membrane provides an accurate representation of hypothalamic temperature. It is less invasive, has a short response time and correlates well with oesophageal temperature. But it does not allow continuous measurements.
❓What is the best method for CONTINUOUS measurement of core temperature?
✔️Blood temperature measurement using a pulmonary artery flotation catheter
❓What are the factors reducing the accuracy of Rectal temperature measurement?
✔️Rectal temperature is influenced by heat generated from gut flora, the cooling effect of blood returning from the lower limbs and the insulation of the probe by faeces. It is normally about 0.5–1.0 ° C higher than core temperature and has a slow response time.
❓Can you say an e.g. of utilising the temperature gradients existing between different sites of the body for clinical advantage?
✔️The gradient between a skin temperature and a core temperature can be used as a marker of peripheral perfusion.