Category Archives: Critical Care
Initiation Strategies for Renal-Replacement Therapy in the Intensive Care Unit — NEJM
Mild TBI – Warning discharge instructions
Pressure Injury Prevention Points
VBG versus ABG
OVERVIEW
Venous blood gases (VBG) are widely used in the emergency setting in preference to arterial blood gases (ABG) as a result of research published since 2001
The weight of data suggests that venous pH has sufficient agreement with arterial pH for it to be an acceptable alternative in clinical practice for most patients
Nevertheless acceptance of this strategy has been limited by some specialties and maybe inappropriate in some settings; for instance there is no data to confirm that this level of agreement is maintained in shock states or mixed acid-base disturbances
Clinically acceptable limits of agreement for blood gas parameters remains poorly defined
ARTERIAL BLOOD GAS PROS AND CONS
Advantages
gold standard test for determining the arterial metabolic millieu (pH, PaCO2, HCO3)
can determine PaO2
Disadvantages
pH, PCO2 (if normocapnic), HCO3 and base excess from a VBG are usually adequate for clinical decision making
SpO2 is usually sufficient for clinical decision making unless pulse oximetry is unreliable for other reasons (e.g. shock state, poor pick up)
painful (should be performed with local anaesthetic in conscious patients)
increased risk of bleeding and hematoma
risk of pseudo aneurysm and AV fistula
infection
nerve injury
digital ischemia
injury to staff
delays in care
serial exams may be needed
venous sampling may better represent the tissue milieu
CORRELATION BETWEEN VBG AND ABG
pH
Good correlation
pooled mean difference: +0.035 pH units
pCO2
good correlation in normocapnia
non-correlative in severe shock
100% sensitive in detecting arterial hypercarbia in COPD exacerbations using cutoff of PaCO2 45 mmHg and laboratory based testing (McCanny et al, 2012), i.e. if VBG PCO2 is normal then hypercapnia ruled out (PaCO2 will be normal), though this conflicts with the meta-analysis by Byrne et al 2014 (see below)
correlation dissociates in hypercapnia – values correlate poorly with PaCO2 >45mmHg
Mean difference pCO2 +5.7 mmHg (wide range in 95%CIs among different studies, on the order of +/-20 mmHg)
A more recent meta-analysis by Byrne et al, 2014 found that the 95% prediction interval of the bias for venous PCO2 was −10.7 mm Hg to +2.4 mm Hg. They note that in some cases the PvCO2 was lower than the PaCO2. The meta-analysis had considerable heterogeneity between studies which limits the reliability of its conclusions.
HCO3
Good correlation
Mean difference −1.41 mmol/L (−5.8 to +5.3 mmol/L 95%CI)
Lactate
Dissociation above 2 mmol/L
Mean difference 0.08 (-0.27 – 0.42 95%CI)
Base excess
Good correlation
Mean difference 0.089 mmol/L (–0.974 to +0.552 95%CI)
PO2
PO2 values compare poorly
arterial PO2 is typically 36.9 mm Hg greater than the venous with significant variability (95% confidence interval from 27.2 to 46.6 mm Hg) (Byrne et al, 2014)
DIABETIC KETOACIDOSIS
VBG can be used to guide management in preference to ABG (Ma et al, 2003)
VBG correlated with ABG well
Mean difference in pH -0.015 ± 0.006 units [95% CI]
ABG pH changed treatment or disposition in 2.5% cases compared to VBG pH
WHEN IS ABG NECESSARY?
ABG may be necessary:
to accurately determine PaCO2 in severe shock
to accurately determine PaCO2 if hypercapnic (i.e. PaCO2 >45 mmHg)
to accurately determine arterial lactate >2mM (rarely necessary)
In general, ABGs rarely need to be performed unless an arterial line is in place (for arterial blood pressure monitoring and ease of blood sampling)
References and Links
1. Byrne AL, Bennett M, Chatterji R, Symons R, Pace NL, Thomas PS. Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis. Respirology. 2014 Jan 3. doi: 10.1111/resp.12225. [Epub ahead of print] PubMed PMID: 24383789. [Free Full Text]
2. Kelly AM. Review article: Can venous blood gas analysis replace arterial in emergency medical care? Emerg Med Australas. 2010 Dec;22(6):493-8. doi: 10.1111/j.1742-6723.2010.01344.x. Review. PubMed PMID: 21143397. [Free Full Text]
3. Kelly AM, McAlpine R, Kyle E. Venous pH can safely replace arterial pH in the initial evaluation of patients in the emergency department. Emerg Med J. 2001 Sep;18(5):340-2. PMID 11559602
4. Koul PA, Khan UH, Wani AA, Eachkoti R, Jan RA, Shah S, Masoodi Z, Qadri SM, Ahmad M, Ahmad A. Comparison and agreement between venous and arterial gas analysis in cardiopulmonary patients in Kashmir valley of the Indian subcontinent. Ann Thorac Med. 2011 Jan;6(1):33-7. PMID 21264169
5. Ma OJ, Rush MD, Godfrey MM, Gaddis G. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med. 2003 Aug;10(8):836-41. PMID 12896883
6. McCanny P, Bennett K, Staunton P, McMahon G. Venous vs arterial blood gases in the assessment of patients presenting with an exacerbation of chronic obstructive pulmonary disease. Am J Emerg Med. 2012 Jul;30(6):896-900. PMID 21908141
7. Middleton P, Kelly AM, Brown J, Robertson M. Agreement between arterial and central venous values for pH, bicarbonate, base excess, and lactate. Emerg Med J. 2006 Aug;23(8):622-4. PMID16858095
8. Tricia M McKeever et al : Using venous blood gas analysis in the assessment of COPD exacerbations: a prospective cohort study –
Thorax doi:10.1136 thoraxjnl-2015-207573
Web resources:
1. ALIEM — Paucis Verbis Card: VBG versus ABG (2012)
2. FET — Venous and Arterial Blood Gas Analysis in the ED by Anne-MArie Kelly (2012)
3. FET — Can a Venous Blood Gas Substitue for an Arterial Blood Gas by Jason Chu (2013)
4. LITFL – VBG versus ABG
Posted from WordPress for Android – Google Nexus 5
https://www.facebook.com/MedicalGeek
https://in.groups.yahoo.com/neo/groups/only4medical/
Five things physicians & patients should consider
Posted from WordPress for Android – Google Nexus 5
https://www.facebook.com/MedicalGeek
https://in.groups.yahoo.com/neo/groups/only4medical/
NHLBI ARDS Network TRIALS
The NHLBI ARDS Network enrolled 5,527 patients across ten randomized controlled trials and one observational study.
Ketoconazole for ALI/ARDS (KARMA)
Mar 1996 – Feb 1998
The first clinical trial completed by the Network was a randomized, controlled trial of Ketoconazole versus placebo in patients with acute lung injury and ARDS. It enrolled 234 participants.
- KARMA Protocol
- Ketoconazole for Early Treatment of Acute Lung Injury and Acute Respiratory Distress Syndrome: A Randomized Controlled Trial. JAMA. 2000;283(15):1995-2002. DOI: 10.1001/jama.283.15.1995.
- ClinicalTrials.gov combined listing for early ARDSNet studies
- BioLINCC combined listing for ARMA/KARMA/LARMA
Lower Tidal Volume Trial (ARMA)
Mar 1996 – Jul 1999
The ARMA study was a randomized, controlled multi-center 2×2 factorial study consisting of a drug treatment (Ketoconazole vs. placebo) and a ventilation strategy (6ml/kg tidal volume vs. 12ml/kg tidal volume). It enrolled 861 participants.
- ARMA Protocol
- Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N Engl J Med 2000; 342:1301-1308. DOI: 10.1056/NEJM200005043421801
- ClinicalTrials.gov combined listing for early ARDSNet studies
- BioLINCC combined listing for ARMA/KARMA/LARMA
Lisofylline for ALI/ARDS (LARMA)
Feb 1998 – Jun 1999
The LARMA study was a randomized, double-blind, placebo-controlled multi-center study with where each patient was randomized between Lisofylline and Placebo. It was designed to test whether the administration of lisofylline early after the onset of ALI or ARDS would reduce mortality and morbidity. It was also conducted in a 2×2 factorial in the later stages of the ARMA trial. It enrolled 236 participants.
- LARMA Protocol
- Randomized, placebo-controlled trial of lisofylline for early treatment of acute lung injury and acute respiratory distress syndrome. Crit Care Met. Jan 2002; 30(1): 1-6. ISSN: 0090-3493
- ClinicalTrials.gov combined listing for early ARDSNet studies
- BioLINCC combined listing for ARMA/KARMA/LARMA
Late Steroid Rescue Study (LaSRS)
Aug 1997 – Nov 2003
The late phase of ARDS is often characterized by excessive fibroproliferation leading to gas exchange and compliance abnormalities. The objective of the LaSRS study was to determine if the administration of corticosteroids, in the form of methylprednisolone sodium succinate, in severe late-phase ARDS, would have a positive effect on this fibroproliferation, thereby reducing mortality and morbidity. It enrolled 180 particpants.
- LaSRS Protocol
- Efficacy and Safety of Corticosteroids for Persistent Acute Respiratory Distress Syndrome; N Engl J Med 2006; 354:1671-1684. DOI: 10.1056/NEJMoa051693
- ClinicalTrials.gov combined listing for early ARDSNet studies
- BioLINCC listing
Higher vs Lower PEEP (ALVEOLI)
Nov 1999 – Mar 2002
The ALVEOLI study was a prospective, randomized, controlled multi-center trial. The objective was to compare clinical outcomes of patients with acute lung injury (ALI)and acute respiratory distress syndrome (ARDS) treated with a higher end-expiratory lung volume/lower FiO2 versus a lower end-expiratory lung volume/higher FiO2 ventilation strategy. It enrolled 549 participants.
- ALVEOLI Protocol
- Higher versus Lower Positive End-Expiratory Pressures in Patients with the Acute Respiratory Distress Syndrome. N Engl J Med 2004; 351:327-336. DOI: 10.1056/NEJMoa032193
- ClinicalTrials.gov combined listing for early ARDSNet studies
- BioLINCC listing
Fluid and Catheter Treatment Trial (FACTT)
Jun 2000 – Oct 2005
The FACTT study was a prospective, randomized, multi-center trial evaluating the use of a pulmonary artery catheter versus a less invasive alternative, the central venous catheter, for the management of patients with acute lung injury (ALI) or acute respiratory distress syndrome (ARDS). It was combined in a 2×2 factorial design with a second study contrasting a conservative and a liberal fluid management strategy in patients with ALI or ARDS. It enrolled 1000 participants.
- FACTT Protocol; see also Footnotes v6 and the algorithm on the tools page.
- Comparison of Two Fluid-Management Strategies in Acute Lung Injury. N Engl J Med 2006; 354:2564-2575. DOI: 10.1056/NEJMoa062200
- Pulmonary-Artery versus Central Venous Catheter to Guide Treatment of Acute Lung Injury. N Engl J Med 2006; 354:2213-2224. DOI: 10.1056/NEJMoa061895
- ClinicalTrials.gov listing
- BioLINCC listing
Albuterol for the Treatment of ALI (ALTA)
Aug 2007 – Sep 2008
A prospective, randomized trial of Aerosolized Albuterol vs. Placebo to test the safety and efficacy of aerosolized beta-2 adrenergic agonist therapy for improving clinical outcomes in patients with acute lung injury. It enrolled 282 participants.
- ALTA Protocol
- Randomized, Placebo-controlled Clinical Trial of an Aerosolized β2-Agonist for Treatment of Acute Lung Injury. Am J Respir Crit Care Med. Sep 1, 2011; 184(5): 561–568. DOI: 10.1164/rccm.201012-2090OC. (or via PMC)
- ClinicalTrials.gov listing
- BioLINCC listing
Early vs. Delayed Enteral Nutrition (EDEN)
Nov 2006 – Mar 2011
Prospective, Randomized Trial of initial trophic enteral feeding followed by advancement to full-calorie enteral feeding vs. early advancement to full-calorie enteral feeding. It enrolled 1000 participants. This trial was originally run as a 2×2 factorial trial with the Omega trial. When the Omega arm was stopped for futility, the EDEN arm continued to completion.
- EDEN-Omega Protocol; EDEN protocol
- Initial Trophic vs Full Enteral Feeding in Patients With Acute Lung Injury: The EDEN Randomized Trial. JAMA. 2012;307(8):795-803. DOI: 10.1001/jama.2012.137. (or via PMC)
- ClinicalTrials.gov listings: as EDEN-Omega; as EDEN
- BioLINCC listing
Omega Nutrition Supplement Trial (Omega)
Nov 2006 – Apr 2009
@TODO A trial of omega-3 fatty acid, gamma-linolenic acid, and anti-oxidant supplementation vs. a comparator. It enrolled 272 participants. It was run as a part of a 2×2 factorial trial with the EDEN study. The Omega arm was stopped for futility.
- EDEN-Omega Protocol
- Enteral Omega-3 Fatty Acid, γ-Linolenic Acid, and Antioxidant Supplementation in Acute Lung Injury. JAMA. 2011;306(14):1574-1581. DOI: 10.1001/jama.2011.1435. (or via PMC)
- ClinicalTrials.gov listing as EDEN-Omega
- BioLINCC listing
H1N1 Registry
Nov 2009 – Jun 2010
A registry created in collaboration with the CDC to track severe cases of H1N1. It enrolled 683 participants.
- H1N1 Registry Protocol
- Critical illness from 2009 pandemic influenza A virus and bacterial coinfection in the United States. Crit Care Med. May 2012; 40(5): 1487–1498. DOI: 10.1097/CCM.0b013e3182416f23. (or via PMC)
- ClinicalTrials.gov listing
- BioLINCC listing
Rosuvastatin vs. Placebo (SAILS)
Mar 2010 – Sep 2013
Statins for Acutely Injured Lungs from Sepsis is a trial of rosuvastatin versus placebo comparator for the treatment of patients with ALI or ARDS. It enrolled 745 participants.
- SAILS Protocol
- Rosuvastatin for Sepsis-Associated Acute Respiratory Distress Syndrome. N Engl J Med 2014; 370:2191-2200. DOI: 10.1056/NEJMoa1401520
- ClinicalTrials.gov listing
- BioLINCC listing
Nutrition in the intensive care unit
Posted from WordPress for Android – Google Nexus 5
https://www.facebook.com/MedicalGeek
https://in.groups.yahoo.com/neo/groups/only4medical/
Antibiotic lock therapy : Summary
Antibiotic lock therapy (ALT) involves instillation of a concentrated antibiotic solution into the catheter lumen with the intention of achieving a drug level high enough to kill sessile bacteria within the biofilm of the catheter. Anticoagulants are often included in the solution and are thought to facilitate antibiotic penetration into microbial biofilm.
For clinically stable children and adults with infections of long-term tunneled central venous catheters and ports due to coagulase-negative staphylococci, gram-negative rods, and vancomycin -sensitive enterococci in whom a decision is made to salvage the catheter, we suggest ALT in conjunction with systemic antibiotics rather than systemic antibiotics alone ( Grade 2B ).
Catheter management options for catheter-related bloodstream infections (CRBSI) include removal, salvage, and exchange over a guidewire. Catheter salvage should not be attempted in the following circuminfections
-Complicated CRBSI
-Severe sepsis or hemodynamic instability
-Persistent bacteremia despite 72 hours of appropriate antibiotic therapy
-Infections caused by S. aureus, P. aeruginosa, fungi, mycobacteria, Bacillus species, Micrococcus species, or Propionibacteria
-Tunnel infections, port abscesses, or exit site infections
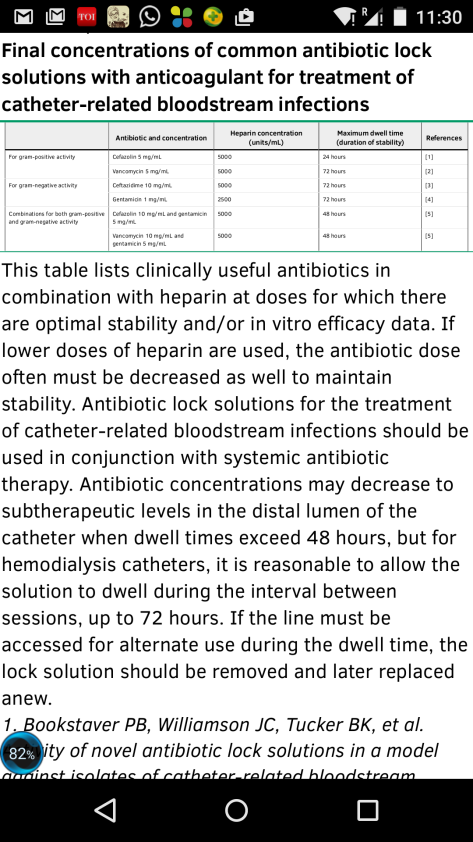
Cefazolin , vancomycin , ceftazidime , and gentamicin are commonly used in ALT and are stable in solution with heparin over a prolonged period of time ( see table ). Specific antibiotic selection for ALT should be guided by culture and susceptibility results when available. We favor a dose in which the final antibiotic concentration exceeds the minimum inhibitory concentration (MIC) of the organism by at least 10administered
For patients receiving ALT, we typically include heparin in the antibiotic lock solution unless there is a contraindication to heparin (eg, heparin-induced thrombocytopenia). For patients with contraindications to heparin, only antibiotics that have been shown be stable and effective when used alone should be administered
Fungal superinfection, systemic toxicities of antibiotics or anticoagulants included in lock solutions, and emergence of antibiotic resistance with failure are potential but not frequently reported adverse effects.
Antibiotic lock solutions should be administered in an amount sufficient to fill and dwell in the catheter lumen when the catheter is not in use. Depending on the need for access, dwell times can range from four to six hours to three days, after which the solution should be withdrawn and discarded.
Infected catheters should be removed in patients who remain febrile 48 to 72 hours after initiating ALT, who have persistently positive blood cultures 72 hours after initiating ALT, or who have signs of sepsis, hemodynamic instability, or metastatic infection.
Posted from WordPress for Android – Google Nexus 5
https://www.facebook.com/MedicalGeek
https://in.groups.yahoo.com/neo/groups/only4medical/
CPR Guidelines – Adults
AHA CPR Guidelines 2010
NOTE: Sequence has changed from airway, breathing, chest compressions (ABC) to chest compressions, airway, breathing (CAB) per the 2010 AHA Guidelines
Untrained lay rescuers should do compression-only CPR; whereas, trained lay rescuers and healthcare providers (HCP) should include compressions and breathing
Compressions
check pulse at carotid
compression landmarks: lower half of sternum, between nipples
compression method: heel of one hand, other hand on top
compression depth: at least 2 inches (5 cm)allow complete chest recoil after each compression
compression rate: at least 100/min compression-ventilation ratio: 30:2 (1 or 2 rescuers)
minimize interruptions in compressions; limit interruptions to <10 seconds avoid excessive ventilation
Airway
head tilt-chin (HCP suspected trauma: use jaw thrust)
Breathing
ventilation with advanced airway: 1 breath every 6-8 seconds (8-10 breaths/min)
asynchronous with chest compressions
about 1 second per breath
visible chest rise
Defibrillation
attach and use AED as soon as available
minimize interruptions in chest compressions before and after shock
resume CPR beginning with compressions immediately after each shock